Navigating the Ethics of AI in Spinal Surgery: Technology vs. Expertise
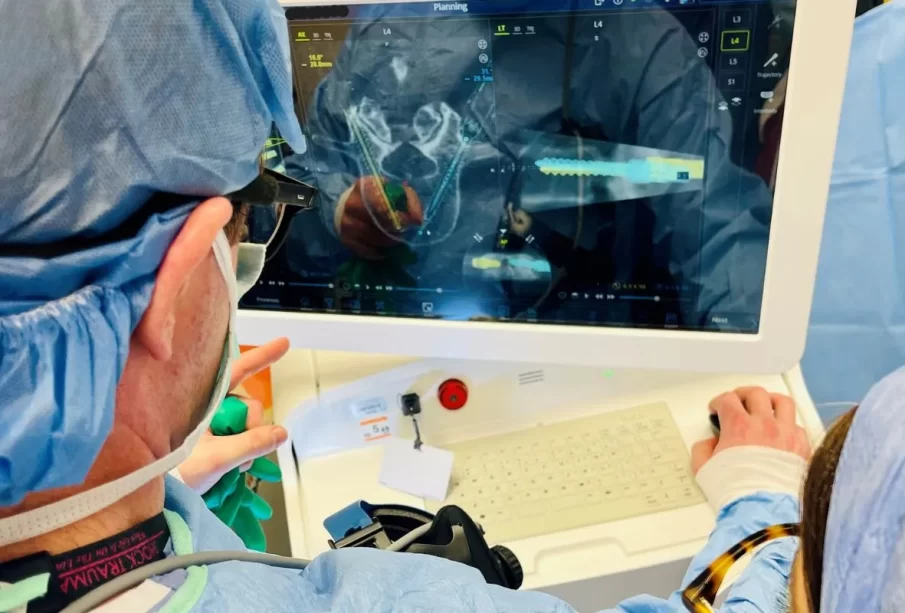
The integration of Artificial Intelligence (AI) into spinal surgery has led to notable advancements in precision, efficiency and patient outcomes. However, as AI becomes increasingly involved in the operating room, it brings ethical considerations to the forefront of surgical practice. Dr. Larry Davidson, an expert in spinal surgery, recognizes that while AI has the potential to enhance spinal surgery significantly, it must be balanced carefully with human expertise to uphold ethical, safe and effective patient care. Achieving this balance is essential to maintaining the trust and integrity of medical practices and ensuring that AI serves as a tool that complements, rather than replaces, human judgment.
The Role of Human Oversight in AI-Guided Surgery
A key ethical concern with AI in spinal surgery is the risk of over-reliance on technology. While AI excels in data analysis and precision, it lacks the adaptive thinking of human surgeons needed for unexpected complications like tissue integrity issues or bleeding. Relying solely on AI could sideline essential human judgment, affecting patient outcomes.
The ideal integration of AI is collaborative—where AI provides data-driven support, but the surgeon retains final decision-making, balancing clinical and ethical factors. This approach safeguards patient safety, promotes responsible AI use and preserves the surgeon’s critical role in care.
Informed Consent and Patient Autonomy
AI’s role in spinal surgery raises important ethical considerations around informed consent and patient autonomy. Patients must fully understand how AI will impact their procedure, including its benefits, limitations and the areas where the surgeon’s oversight remains essential. Transparency is crucial to ensuring patients have the information needed to make informed decisions.
For consent to be meaningful, patients should have the option to accept or decline AI involvement and, if uncomfortable, explore alternative treatments. Respecting patient autonomy and choice builds trust and ensures that AI supports patient-centered care rather than diminishing it.
The Risk of Dehumanizing Care
One ethical dilemma posed by AI in surgery is the potential for dehumanizing patient care. Surgery is not solely a mechanical process; it also involves empathy, effective communication and a deep understanding of each patient’s unique needs and concerns. Spinal surgery can be daunting for patients due to its complexity and the significant impact it has on mobility and quality of life.
While AI can improve the technical precision of surgery, it cannot replace the compassion and understanding provided by a human surgeon. AI lacks the emotional awareness to respond to patients’ concerns, offer reassurance or adapt its communication style to suit individual preferences. Balancing the use of AI with a patient-centered approach is essential for preserving the compassionate care that defines ethical medical practice.
Surgeons play a critical role in ensuring that AI does not overshadow the human connection essential to effective healthcare. While AI handles the technical aspects, surgeons must focus on maintaining open communication with patients, explaining the procedure and addressing any concerns with empathy and understanding. Ethical AI use in spinal surgery involves not only achieving technical accuracy but also preserving the human elements of care—trust, compassion and personalized support.
Accountability and Liability
As AI becomes more prevalent in spinal surgery, questions around accountability and liability become more pressing. In conventional surgery, if an error occurs, the surgeon is typically held accountable. However, in an AI-assisted procedure, the responsibility becomes less clear. If an error occurs based on an AI recommendation, determining whether the fault lies with the surgeon, the AI system or the institution can be challenging.
The lack of clear guidelines around accountability in AI-driven surgeries presents ethical and legal challenges. Surgeons need to maintain full accountability, even when AI is involved, to ensure patient safety and trust. However, holding surgeons solely responsible may be unfair if an error arises from an AI system’s limitations or a flawed algorithm. In such cases, accountability may need to be shared between the surgeon and the AI developers or the institution.
Developing ethical frameworks and policies to address liability in AI-assisted surgeries is crucial. These frameworks should define the roles and responsibilities of each party involved, including the surgeon, the healthcare institution and AI developers. Additionally, guidelines are needed for handling errors or adverse outcomes arising from AI recommendations, ensuring that patients receive fair and just responses when complications occur. Collaboration among medical professionals, legal experts and AI developers will be essential in creating policies that protect patients while enabling responsible AI use in surgical care.
Striking the Right Balance: Human Expertise and AI Support
The ethical use of AI in spinal surgery requires a careful balance between technology and human expertise. While AI has the power to enhance surgical precision and efficiency, it cannot replace the depth of insight and judgment that experienced surgeons bring to the operating room. Ethical use of AI means that technology should serve as a supportive tool, empowering surgeons to make more informed, accurate decisions without sidelining their skills or judgment.
Dr. Larry Davidson says, “AI will provide us with the ability to have a total and comprehensive understanding of the patient’s medical history and what sort of spinal interventions would be considered best.”
AI must complement, not replace, the ethical judgment and expertise of skilled surgeons. Surgeons are responsible for integrating AI insights with their clinical understanding to deliver safe, effective care that respects patient rights and dignity. By balancing AI’s technical capabilities with human oversight, the medical community can ensure that AI is used responsibly, enhancing surgical outcomes while upholding the ethical standards that define quality healthcare.
The Path Forward: Ethical AI Integration in Healthcare
As AI technology continues to evolve, its role in spinal surgery will likely expand, offering new possibilities for precision and patient care. However, the ethical challenges surrounding AI must be addressed proactively to ensure it enhances, rather than compromises, the quality of medical care. Moving forward, healthcare institutions will need to establish clear ethical guidelines, provide transparency to patients and emphasize the importance of human oversight in AI-driven surgeries.
Ultimately, the goal is to create a healthcare environment where AI supports patient-centered care, enhancing the capabilities of skilled surgeons while respecting patient autonomy, maintaining empathy and safeguarding accountability. With ongoing collaboration among healthcare professionals, policymakers and AI developers, the integration of AI into spinal surgery has the potential to improve outcomes while preserving the trust, integrity and ethical foundations of medical practice.