Understanding Hernia Removal Surgery and What Patients Should Expect
A hernia isn’t just “a lump.” That’s the surface version. What’s really happening: part of an organ or tissue squeezes through muscle that’s too weak to hold it in. Think of a soft patch in a wall where plaster crumbles and something pokes through. Same principle.
Why the weakness forms—several reasons. Some people are born with it. Others grind their muscles down over years. Heavy lifting. Constant coughing. Straining on the toilet. Pregnancy, too. All of these add stress. Eventually, something gives.
The types? Inguinal, femoral, umbilical, hiatal. Each looks or feels different. Some show up as visible bulges, others hide inside the chest and announce themselves with heartburn. Because of that variety, treatment isn’t cookie-cutter. What works for one patient might not fit another. Which is exactly why doctors talk carefully about hernia removal surgery instead of rushing everyone into the same plan.
When Surgery Moves From Option to Necessity
Here’s the blunt part: hernias don’t heal on their own. The gap in the muscle wall doesn’t seal back up magically. Belts, binders, “resting it”—all temporary fixes. So the real question becomes timing. Some patients live for years with a small hernia. Manageable. They adjust. Then one day, the bulge gets trapped. Tissue strangulates. Blood flow stops. Pain skyrockets. Now it’s an emergency. Doctors have hours, not days, to operate.
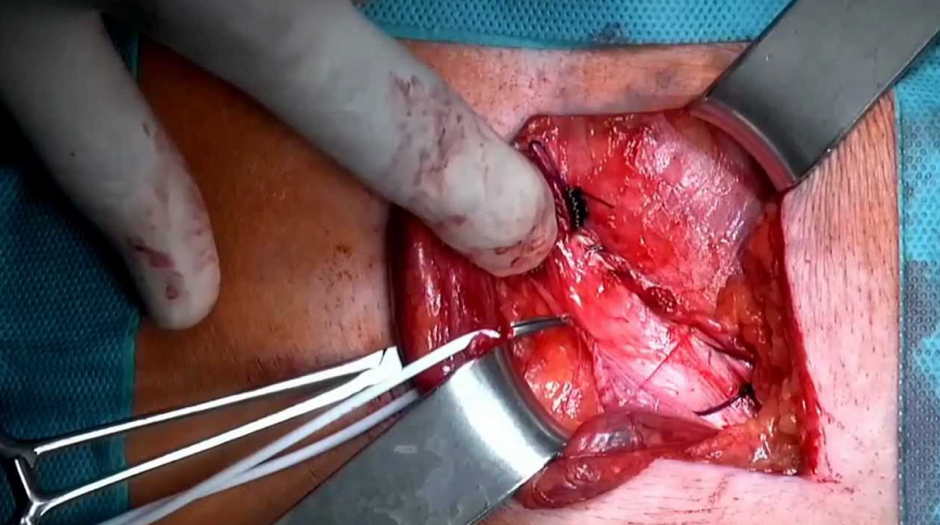
Different Surgical Paths: Open vs. Laparoscopic
Two main approaches exist. Open surgery, the traditional one: one incision, surgeon pushes the tissue back, patches the weak spot, usually with mesh. Tried and tested. But the recovery can stretch longer, with soreness that lingers. Then there’s laparoscopic surgery. Instead of one cut, several tiny entry points. A camera, slim tools, repairs done from the inside. Patients like it because scars are smaller, pain is lighter, and recovery quicker. But—important caveat—it’s not for everyone. Large hernia? Lots of scar tissue from previous operations? Sometimes open is the safer call.
Neither is “better” across the board. It depends. On the patient, the hernia itself, even the surgeon’s expertise.
Preparing for Surgery: More Than Marking a Date
Preparation goes beyond putting the surgery on your calendar. Doctors check medical history, current meds, heart and lung function. Imaging if needed. If you’re on blood thinners, you may need to pause them. Smokers often get a strong nudge to quit, at least temporarily, since nicotine slows healing. Fasting usually starts the night before. No food, no drink. Not everyone realizes why: anesthesia complications are more likely if the stomach isn’t empty.
And there’s the mental part. People who know exactly what will happen—the anesthesia, the grogginess, the soreness, the timeline—recover smoother. Fear, on the other hand, magnifies every ache. Which is why good surgeons explain, not just cut.
What Recovery Really Looks Like
Recovery isn’t a neat, single timeline. One patient says, “I was back at work in a week.” Another struggles for a month.The first days bring soreness, swelling, sometimes bruising. Coughing hurts. Laughing hurts. Simple things—getting out of bed, tying shoes—feel awkward. Walking is encouraged early, but lifting anything heavier than a jug of milk? Strictly no. For weeks.
By two weeks, many are back to desk jobs. But physical jobs—construction, warehouse work, athletes—often need six weeks or more. The danger is trying to “push through.” That risks tearing the repair before it’s strong enough. Which means another surgery, something nobody wants.
Risks, Recurrence, and Realities
No surgery is risk-free. Hernia repairs can bring infection, bleeding, anesthesia complications. Rare, but real. Then there’s mesh. Modern meshes are much safer than older versions, yet patients still worry. It’s worth asking your surgeon what type they’ll use, how often they’ve worked with it, what outcomes they see. Transparency matters.
Recurrence—that fear of it coming back—lingers. The truth: recurrence rates today are lower, thanks to better techniques. But risk isn’t zero. Weight gain, chronic coughing, or constant straining can push the repaired wall again. Lifestyle matters as much as surgery. Compare that with the risk of doing nothing. Untreated hernias can strangulate, obstruct, and land patients in the ER. At that point, options are fewer, and recovery is harder. Which is why, for most, timely hernia removal surgery is the safer, smarter choice.
Life After Repair
Most patients say the same thing afterward: relief. The constant bulge, the dull ache, the worry every time they bend down or carry groceries—it’s gone. Suddenly, they move without hesitation. Confidence comes back. But the repair isn’t invincible. The body still needs care. Staying at a healthy weight, strengthening core muscles safely, avoiding unnecessary strain—these steps protect the repair. Think of it as maintenance.
Patients who follow that advice usually do well. Those who don’t sometimes end up back where they started.
Conclusion
A hernia is more than a lump. It’s a structural flaw, one that worsens with time. Living with it may seem manageable, but risks escalate fast. Modern surgery—open or laparoscopic—offers reliable repair, a way back to strength and peace of mind. For those weighing the decision, hernia removal surgery isn’t just treatment. It’s the step that restores safety, comfort, and control.